Since being diagnosed as a type I diabetic at the age of four, my life has been full of highs and lows. Growing up as the youngest among four competitive brothers, my drive to excel in every facet of life was relentless. My diagnosis reshaped my entire outlook, transforming my pursuit of success into a daily struggle within myself. The consequences of losing this battle entailed diminished performance in my academics, athletics, and life. Yet, navigating this daily fight has gifted me invaluable lessons about life and has fostered a deep understanding of my identity and aspirations. I write this with the hopes it will improve your understanding of diabetes management and heighten your awareness of the innovation in diabetes research today.
What is Diabetes?
Insulin is produced by beta cells within your pancreas and is an essential hormone that controls the level of glucose in your blood. Diabetes results from your pancreas’s inability to generate sufficient amounts of insulin. There are two types of diabetes: type I and type II.
In type I diabetes, the body’s immune system mistakenly kills your beta cells, resulting in your body being unable to produce insulin. People with type I diabetes give insulin doses for any food consumed, using either an insulin syringe or an insulin pump. While insulin syringe users will use long-acting insulin for periods when they are not eating, an insulin pump will deliver small hourly doses of insulin known as a “basal rate.” This information will be necessary to understand how data is used to create artificial pancreas systems that could one day make diabetes management practically obsolete.
In type II diabetes, your body can produce insulin naturally, but the amount generated by your beta cells is insufficient for glucose homeostasis. People with type II diabetes commonly manage their health with dieting and exercise, as well as through medication and insulin.
How I Manage My Diabetes
Initially, I used insulin syringes to deliver both short and long-acting insulin. I quickly switched to an insulin pump as it provided improved control over my diabetes management. I could set hourly carb ratios, basal rates, and settings for things such as insulin sensitivity. Carb ratios are the ratio of carbohydrates to a unit of insulin. It is common for your body to have different ratios for different periods of the day. The same is true of insulin sensitivity, as a unit of insulin may lower your blood sugar by 50 mg/dL in the morning but 40 mg/dL in the evening.
The Continuous Glucose Monitor (CGM) revolutionized diabetes management by providing real-time insights, and empowering individuals to make informed decisions about insulin dosing, dietary adjustments, and more. Before owning a CGM, I regularly pricked my finger to test my blood sugar throughout the day. With my CGM, I can easily track trends in my blood sugars and make quick adjustments.
Today, I use a Dexcom G6 Continuous Glucose Monitor with my Tandem t:slim X2 Insulin Pump. Both systems work together in what is called a “closed-loop system.” If my CGM registers that my blood sugar is low, my pump will reduce my basal rate or halt insulin delivery completely until my blood sugar rises to an appropriate level. If my CGM registers that my blood sugar is high, my pump will increase my basal rate until my blood sugar drops to a proper level. This is incredibly impactful when I sleep. A diabetic’s biggest blindspot is in the middle of the night when they are not conscious. Previously, I had to be cautious about eating before bedtime, and carefully balance insulin doses to avoid potential complications. Now, with the aid of my pump and CGM, even if I consume something before bed and miscalculate the insulin dosage, the pump’s adaptive features help maintain stable blood sugar levels overnight. This advancement holds significant importance for diabetic children since their growth and development peak during sleep. It offers a safety net, ensuring their health remains optimized, even if they indulge in a late-night snack or face insulin discrepancies. Figure 1 displays an example of how a closed-loop system operates to improve blood sugar management.
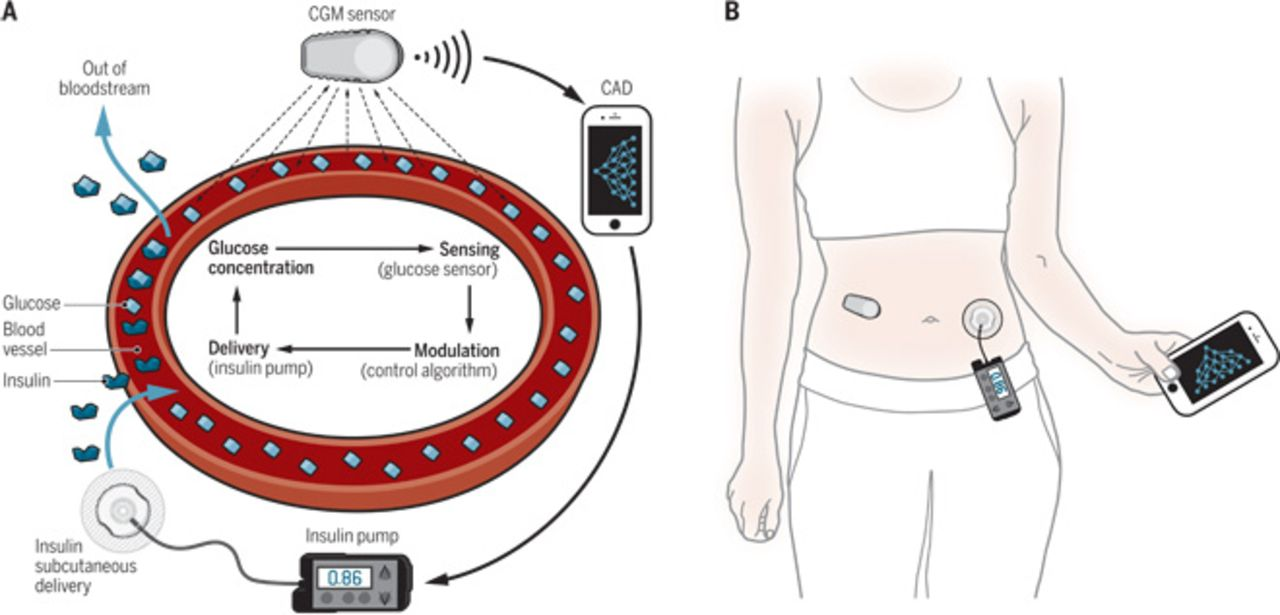
Figure 1: Example Diabetic Closed-Loop System
Charlotte K. Boughton, Roman Hovorka, Advances in artificial pancreas systems. Sci. Transl. Med. 11, eaaw4949 (2019). DOI:10.1126/scitranslmed.aaw4949
Data and The Future of Diabetes Management
As a type I diabetic, my life is full of data. It equips me with the power to care for myself to the best of my ability. The closed-loop system has taken loads of pressure off me and my diabetes management. As a data scientist, I am incredibly excited about where continued innovation in healthcare spaces will take us. Since childhood, I have heard tales of the infamous “Bionic Pancreas.” A device that can deliver both insulin and glucagon to manage a patient’s diabetes fully in a true “closed-loop system.”
On May 22, 2023, Beta Bionics announced FDA clearance and commercialization of the iLet Bionic Pancreas. In their release, they state their system requires “No carb counting*, no corrections, no calculating boluses” and “only needs your body weight to get started.” Beta Bionics iLet Bionic Pancreas represents a remarkable milestone in diabetes management research and innovation. UT Southwestern’s study reported that “results showed that patients using the bionic pancreas improved their glycated hemoglobin measurements to 7.3% from 7.9% on average.” Furthermore, “bionic pancreas group participants spent 11% more time, about 2.5 hours per day, within the targeted blood sugar range compared to the control group.” They later detailed the impact, stating, “these results suggest this new technology could significantly improve blood sugar control among those with type 1 diabetes, helping them avoid complications frequently associated with this disease, including heart attack, stroke, nerve damage, and blindness.” As a participant in UNC Hospital’s clinical trials of Beta Bionics iLet Bionic Pancreas, the potential of the device gives me immense hope and excitement for the future. It is important to recall that this is the first bionic pancreas with FDA approval. The current FDA approval is for an insulin-only iLet Bionic Pancreas; however, trials are currently being performed to test dual-hormone systems capable of delivering both insulin to lower glucose levels and glucagon to raise blood glucose levels.
My time at the Institute for Advanced Analytics at North Carolina State University has deepened my comprehension of data analytics and storytelling, pivotal skills that have transformed me into a more adept analyst of my own health.
Through this experience, I’ve gained a better understanding of the cause-and-effect dynamics of my diabetes management and a heightened appreciation for the immense effort underlying technological innovation today. I am enthusiastic about applying my newly heightened skills to the abundance of data innovation around me in my career post-graduation. Just as I was inspired by the tales of the ‘Bionic Pancreas’ during my youth, I eagerly anticipate the future emergence of other life-changing innovations in healthcare and beyond. Being part of the process of making these advancements a reality fills me with excitement and purpose, and I can’t wait to contribute to this transformative field firsthand.
Positive Mental Attitude (PMA)
I attribute much of the success I’ve experienced at the institute and in my life to maintaining a Positive Mental Attitude (PMA), and I encourage you to cultivate one too. I can not overstate the impact it has had on my life. I first learned about PMA at a diabetes camp, and it is the most essential life lesson I have ever known. Everyone experiences adversity differently, and as a person with diabetes, you have to multitask every activity with the management of your health. Some days, you might do everything wrong and feel physically terrible because of it. My accomplishments are deeply rooted in the unwavering support I have received from friends and family, coupled with a steadfast commitment to maintaining a Positive Mental Attitude.
As you continue your diabetes education, I implore you to foster welcoming and supportive environments for those diagnosed as they continue their daily battle for improved diabetes management. Fueled by relentless advancements in data systems and a resilient mindset, I stand prepared to conquer any obstacle. This journey is not mine alone; it is a testament to resilience and adaptability for us all. Together, let us embrace the future with unwavering optimism and the certainty that challenges can be overcome!
Columnist: Casey Mook